Table of Contents (sections numbered below)
- How COVID-19 has Affected the Ongoing Opioid Crisis
- Addiction Recovery Hindered by Coronavirus
- Isolation Increased the Risk of Overdose Deaths
- Elements of Recovery Inhibited by COVID-19
- Virtual Treatments
- What Can Be Done To Prevent More Overdoses
- What is CDC Doing?
- Improving Patient’s Safety
- Collaborating With Public Safety
- Collecting and Analyzing Data
- Educating the Public
- Helping States to Implement Effective Strategies
- What We Need To Do Now
Even before Covid-19 arrived, the United States was already afflicted with an opioid crisis that has only continued to get worse over the past two decades. In fact, more than 400,000 people have died from a drug overdose involving opioids in the U.S. since 1999. Sadly, the pandemic only accelerated the problem as mandated isolation caused a “perfect storm” for those struggling with substance use disorder. With limited social and family interactions, and many losing their jobs, the pandemic itself is depressing and anxiety provoking. Unfortunately, these are all stimuli that can increase stress to the psyche of someone who has an addiction.
How COVID-19 has Affected the Ongoing Opioid Crisis
Increases in overdoses are not surprising during dark times. Assistant professor of psychiatry at Yale University, Ayana Jordan, pointed out that extreme isolation, financial stress, and grief—all drive progression to addiction and escalate the likelihood of overdose. As Covid-19 became more widespread, these emotions were felt by most, and in some cases could even push people recovering from addiction right back into substance use. Furthermore, lack of access to treatment centers and support systems only added “fuel to the fire” for this vulnerable population.
Addiction Recovery Hindered by Coronavirus
The need to be isolated to stay safe from Covid-19 prevented people suffering with addiction from meeting with their peer-support groups, which are vital for those in recovery—as they provide enormous emotional support. Consequently treatment clinics experienced a significant drop in patient volume, depleting crucial revenue for operations. To “add insult to injury”, these addiction recovery centers were simultaneously blindsided by an increase in overhead from new Coronavirus safety measures. These painful new realities have made it near impossible for many of these safe havens to stay afloat during the pandemic—further limiting patients access to necessary treatment.
Isolation Increased the Risk of Overdose Deaths
Stress and anxiety are known as universal triggers for drug use, which also happen to be two of those most common emotional responses that come from isolation. Even worse, with a spike in people using drugs alone during the pandemic, more overdose deaths have taken place—as it created a scenario in which no one was nearby to call 911 during those potentially life-saving final minutes of their lives. Moreover, with less ICU beds available during the pandemic, it has been incredibly challenging for hospitals to accommodate patients battling an overdose—causing even more fatalities.
Elements of Recovery Inhibited by COVID-19
Many of the key elements of addiction recovery were halted by the pandemic. Including (but not limited to);
- Health: Incorporating exercise in one’s daily routine is an important component of recovery—as it supports physical and emotional well-being. However, the pandemic forced those in much need of their local gym to stay home.
- Purpose: The impact of Covid-19 led to unprecedented unemployment in many parts of the US—leaving many without a sense of purpose. Additionally, the correlation between economic distress, unemployment, and a rise in drug overdoses is well documented.
- Community: To fully recover, one needs support, love, and a sense of community. But social distancing quickly resulted in nearly the total-disappearance of live events, and gatherings—disrupting the road to recovery for many.
Virtual Treatments
Although virtual treatment seems logical to healthy individuals, those who suffer from addiction generally find it more difficult to pivot and change counselors. This sudden predicament catapulted fear and anxiety levels for those in a recovery program, transitionally deepening emotional pain and heightening the cravings of opioid and drug use.
What Can Be Done To Prevent More Overdoses
Thankfully some policies have already been put in place by the federal agencies to increase access to take-home doses of medication used to treat Opioid Use Disorder (OUD) and also to expand Telehealth access for addiction treatments. Opening the doors to essential services will allow us to discover new ways to care for people going through this relentless journey. As vaccines continue to roll-out as well, many much needed and familiar recovery programs will soon again be available. In the meantime, additional support can be accessed immediately on our website or you call us now for help.
What is CDC Doing?
The CDC issued a health advisory to medical and public health professionals, first responders, and other community partners—recommending the following actions to implement as soon as possible:
- Expanding distribution and usage of Naloxone.
- Building awareness of overdose prevention education.
- Increasing accessibility and availability of recovery treatments.
- Proactively seeking to help those at the highest risk of overdose as early as possible.
- Using improved detection technology to locate overdose outbreaks and facilitate a more effective response.
The CDC is assessing addiction & overdose data to understand trends and collaborating with funded jurisdictions to provide assistance where needed. This vital information is also sent to public health agencies and used to identify potential strategies on ways to navigate the new obstacles created by the pandemic.
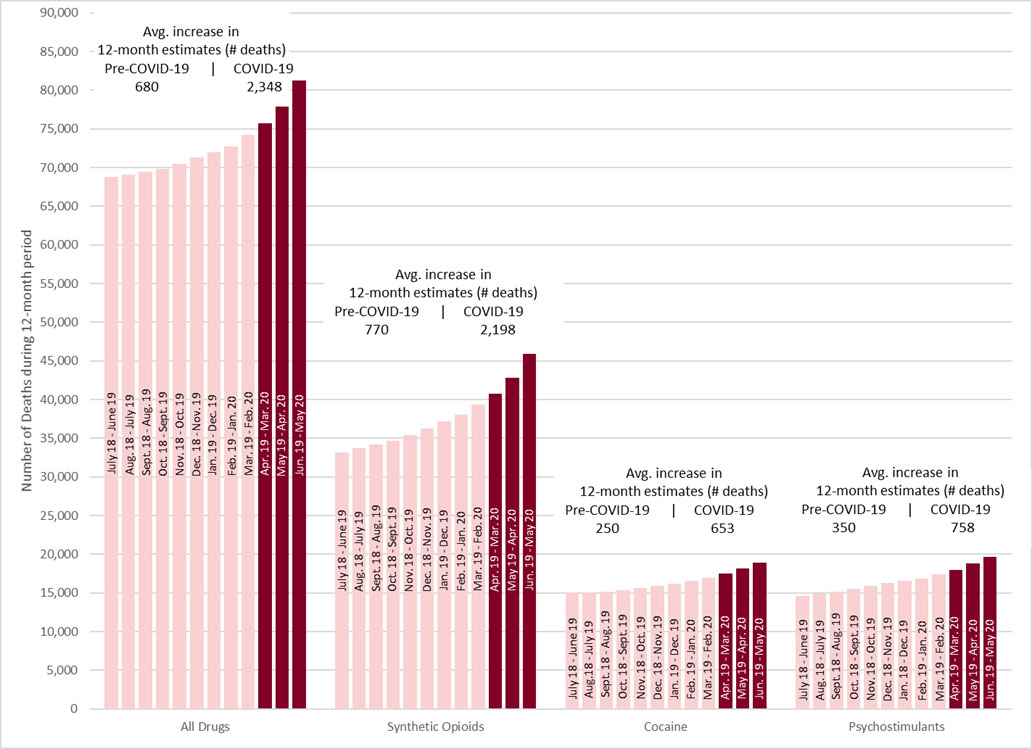
Figure 1: Shows drug overdose deaths in the US from June 2019 – May 2020 and COVID-19 spike:
Below are some of the strategies that were developed to prevent opioid overdose and addiction:
Improving Patient’s Safety
The first way to ensure patient safety is by reducing harmful exposure to opioids and treating addiction alongside health care facilitators. This approach provides patients access to safer, more effective treatments. Ultimately, improved safety can be achieved by considering the following:
- Determining the right time to initiate or continue opioids for chronic pain
- Selection of therapy such as non-pharmacological therapy, nonopioid pharmacologic therapy, or opioid therapy as a last result
- Establishing treatment goals accordingly
- Thoroughly understanding potential risks and benefits of treatment
- Opioid selection, dosage, duration, follow-up, and discontinuation
- Exact duration of the treatment enforced
- Proper dosage followed
- Doctors selecting long-acting opioids, immediate-release or extended-release
- “Hand-held” discontinuation of opioid therapy
- Addressing harms and assessing potential risks of opioid use
- Routine urine-drug testing
- Arranging and managing treatment for opioid use disorder (OUD)
- Education of risk factors for opioid-related harms and ways to avoid patient risks
- Analyzing prescription drug monitoring program (PDMP) data
Collaborating With Public Safety
CDC has developed new alliances with law enforcement to tackle the growing illicit opioid problem. The agency has partnered in innovative ways with public safety and leads prevention strategies in High Intensity Drug Trafficking Areas. Enhanced communication and collaboration between these agencies improves data sharing, surveillance, and the targeting of interventions.
First responders including the fire department, police, and paramedics are on the frontlines of the epidemic. As such, they are often in a position to save lives with timely administration of naloxone. Transitionally, they may also unknowingly come into contact with opioids from time-to-time, including illicitly manufactured fentanyl. Thankfully the CDC provides guidance for these first responders exposed to synthetic opioids when attending to medical calls, crime scenes, or even during drug raids.
Collecting and Analyzing Data
Data collection is essential for developing cutting-edge strategies. With this in mind, CDC plans to improve their data quality by leveraging modern technology to track major trends more accurately. These advancements will forge improved response tactics to grapple with new challenges created by the epidemic. The data will also help to analyze opioid-related overdoses and identify problematic areas.
CDC’s Data and Injury Center identifies overdoses for these four categories of opioids:
- Methadone, a synthetic opioid used to treat pain. It can also aid narcotic drug addiction.
- Heroin, an illegal and highly addictive opioid drug.
- Natural opioids, such as pain medications like morphine and codeine.
- Synthetic opioids, such as fentanyl, are a class of drugs that relieve pain like opiates.
Educating the Public
CDC has prepared a campaign to make people aware of the addiction risks and potential danger of prescription opioids. It includes real-life stories from people that were severely harmed by opioids.
The campaign’s goals include:
- Expanding awareness about how dangerous and addictive prescription opioids can be.
- Spreading the message that help is readily available, if and when needed.
- Providing support from start-to-finish of their recovery process.
CDC also filmed and captured more real stories to add to the awareness campaign. The new ads focus on audiences heavily impacted by the opioid overdose epidemic. Local health departments and community organizations plan to use the campaign materials to raise awareness about the risks of prescription opioids.
Helping States to Implement Effective Strategies
While ensuring patients have access to safer pain treatment, the CDC is also working with States to provide funding, and useful information to further understand the risks of opioid use disorder, prevention from overdoses, and mortality.
CDC also plans to award states up to $1 million to excel prevention in four significant areas:
- Policy Evaluation
- Community health system intervention
- Rapid response
- Bolstering PDMP
What We Need To Do Now
The United States is facing two concurrent public health emergencies, the pandemic, and the opioid crisis. The opioid epidemic was already growing, but COVID-19 has made it even worse.
This dual crisis continues to have devastating effects on individuals, families, and communities across the US. It should be the goal of our Nation to reduce opioid misuse and overdoses through the implementation of evidence-based treatments and recovery support services.
If you or a loved one needs support, or you would like to learn more about how you can help, please contact us for more information.
